
Hysterectomy


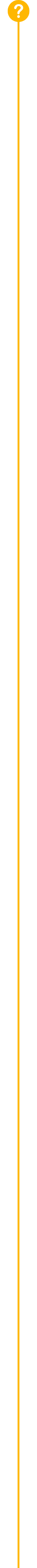
A standard hysterectomy is the removal of the cervix and the uterus. The ovaries, which make female hormones, are often left in place.
What is a hysterectomy?
A hysterectomy is a surgery performed to remove a woman’s uterus and cervix. A supracervical hysterectomy only removes the uterus. In all cases, menstruation stops and a woman loses the ability to bear children.
Are hysterectomies common?
Extremely. According to the CDC, more than 500,000 women undergo a hysterectomy every year and one in three will have a hysterectomy by age 60. (1)
What are the functions of the female reproductive organs, and which organs are removed during a hysterectomy?
A hysterectomy removes a woman’s uterus and cervix only, and does not include removal of the ovaries. The removal of the ovaries and tubes is called an oopherectomy.
Because hormone production is sourced at the ovaries, menopause or “the change” does not occur after a hysterectomy is performed. This means that menopausal symptoms such as hot flashes, night sweats, mood swings, anxiety, depression, osteoporosis (bone loss), vaginal dryness, and sexual dysfunction will not usually occur with a hysterectomy.
About Your Body
- The cervix is the lower, narrow part of the uterus (womb) and forms a canal that opens into the vagina, which leads to the outside of a woman’s body.
- Fallopian tubes are two, thin muscular channels in the female reproductive system that connect the ovaries to the uterus. They create the path that the eggs use to travel from the ovaries to the uterus.
- The ovary is one of a pair of female reproductive glands located in the pelvis, one on each side of the uterus. Ovaries produce eggs and female hormones.
- The uterus, often called the womb, is a muscular organ in the lower part of a woman’s body in which a fertilized egg implants and develops into a fetus.
- The vagina is a muscular passage that connects the cervix with the outside of the body.
Why would a woman need to undergo a hysterectomy?
3 primary reasons include:
- Removal of fibroids, which are non-cancerous tumors
- Treatment of endometriosis, the growth of the uterine lining outside of the uterus
- Resolve uncontrolled bleeding caused by adenomyosis, cancer or pelvic organ prolapse
What are the different ways that a hysterectomy is performed?
Although many women (45%) still undergo invasive open abdominal hysterectomy in a hospital setting, new forms of laparoscopic hysterectomy are less invasive, leave little visible scarring, have a shorter recovery period, and allow the patient to go home the same day.
Today, approximately one-third of U.S. hospitals perform all hysterectomies through open surgery.
Hysterectomy Techniques
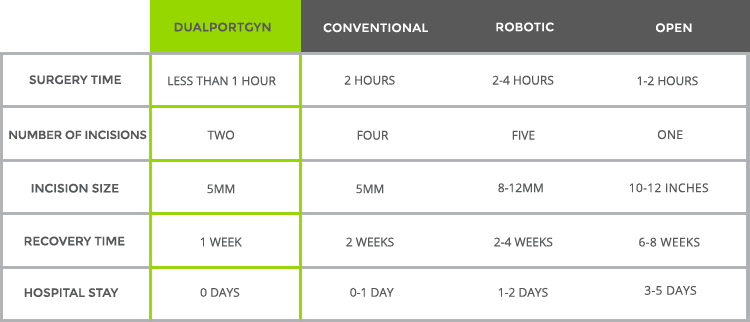
- Open abdominal hysterectomy, or a “traditional” hysterectomy is performed in a hospital and entails removing a woman’s uterus and cervix through an eight inch incision at the bikini line – similar to the incision for a Cesarean Section. Open procedures usually require staying in the hospital 3-5 days and a recovery time of 6-8 weeks.
- Total vaginal hysterectomy entails removing the uterus and cervix through an incision deep within the vagina. Vaginal hysterectomies involve a shorter time in the hospital and have a faster recovery than an open abdominal hysterectomy. However, if the woman’s uterus is enlarged or there is scar tissue in the pelvis from prior surgery vaginal hysterectomy may not be possible. This procedure is performed without any visual assistance in the abdominal cavity.
- Total laparoscopic hysterectomy is a minimally invasive procedure, which removes the uterus and cervix, and requires three to four, 5 millimeter incisions in the abdomen. After surgery, patients have a much quicker recovery than with an open abdominal hysterectomy, usually going home the same day or staying overnight in the hospital.
Note: Additionally, women can select to have a laparoscopic supracervical hysterectomy, during which the uterus is removed laparoscopically, but the cervix is left (Supra means above). Three to four incisions are used, ranging in size from 5mm to 10mm. - Robotic hysterectomy removes the uterus and cervix through laparoscopic incisions in the abdomen. Also performed in a hospital, a robotic hysterectomy typically involves five, 8-12 millimeter incisions in the abdomen. It may also take longer to conduct the surgery, which means the woman may be under anesthesia longer and increase the surgical risks.
- Laparoscopically assisted vaginal hysterectomy (LAVH) uses a laparoscope to guide the removal of the uterus through the vagina. Through this surgical procedure, three to five ports are located in the pelvis, ranging in size from 5 to 10 millimeters. Although the scars, pain and recovery time from LAVH are usually significantly less than an abdominal surgery, LAVH can be a longer operation and more expensive than a vaginal hysterectomy and other minimally invasive laparoscopic surgical options.
- DualPortGYN hysterectomy, a pioneering new procedure, uses only two, 5 millimeter incisions to remove the uterus and cervix with the use of laparoscopy. One incision is placed at the belly button and the other is at the C-Section line. With these incisions, large fibroids and masses can be removed safely in less than one hour.
How does DualPortGYN work?
- Clearer view – DualPortGYN uses a technique known as retroperitoneal dissection (RPD), originally developed to remove cancerous tissue. By going behind (retro) the lining (peritoneal), the surgeon completely visualizes all of the anatomy of the pelvis, and avoids complications such as excessive bleeding and injury to the ureter and bladder. RPD allows surgeons to map the organs and arteries in the pelvis, much like a GPS system, reducing the time of the procedure and avoiding injury to the pelvic structures.
- Fewer complications – DualPortGYN hysterectomy also uses a technique called uterine artery ligation (UAL). UAL minimizes blood loss, which can reudce complication rates and improve recovery times.
- More convenience – In many situations, the surgery is performed on an outpatient basis allowing patients to go home the same day and return to most normal activity in approximately one week.
What are the major risks associated with a hysterectomy?
As with any other type of surgery, hysterectomy is associated with certain risks, but the potential for complications depends on the type of procedure. In women undergoing an open abdominal hysterectomy, risks include blood clots, infection, excessive bleeding, adverse reactions to anesthesia, and in some instances, damage to the ureter (which is the tube that transports urine from the kidney to the bladder), bladder, rectum or other pelvic structures during surgery. When this happens, additional corrective surgery is required.
Compared with abdominal hysterectomy, laparoscopic surgery has a lower risk of infection. However, when surgeries are performed by physicians that do not specialize in GYN surgery, there is the also potential to injure the surrounding vital structures, again, requiring corrective surgery. Other risks include excessive blood loss, surgical site infections, and the potential for the closure of the top of the vagina coming undone.
How long is recovery?
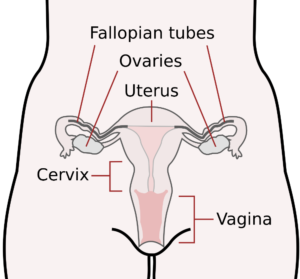
Because there are many types of hysterectomy, recovery times vary. It can take from one week to 6-8 weeks to recover depending on the procedure. This chart details the average recovery time for a variety of hysterectomy techniques.
What kind of scars will I have?
The number and size of the incisions involved in the surgery determines the amount of scarring. This chart details the location, number and size of incisions by hysterectomy procedure.
What should I ask my doctor if a hysterectomy is prescribed?
Before undergoing surgery, you will likely have many questions for your doctor or OB-GYN. Below are some recommended questions to ask – and background information to help you weigh the answers. You can also download a printable version of these questions.
HOW WILL THE SURGERY BE PERFORMED?
Sixty percent of all the hysterectomies performed in the U.S. are still open abdominal surgeries. This procedure can result in severe pain, higher complication rates, and a longer recovery period than new minimally invasive procedures. Other clinics use robotics, which require more incisions and more scarring. If your physician recommends these options, consider seeking a second opinion before agreeing to surgery.
HOW MANY TIMES HAS THE PHYSICIAN PERFORMED THIS PROCEDURE?
When it comes to any form of surgery, training, skill and practice matter, which is why GYN surgeons who specialize in minimally invasive surgery are the most qualified. The reality is that OB-GYNs are highly skilled obstetric practitioners, but very few perform GYN surgeries often enough to be surgical specialists. This is borne out by studies, which find that GYN surgery is commonly a secondary component of what an OB-GYN does.
WHAT HAVE OTHER PATIENTS EXPERIENCED AFTER THIS PROCEDURE?
Robotic, open and conventional laparoscopic hysterectomies can lead to longer recovery times, increased blood loss and larger scars than newer procedures. Make sure your surgeon is trained in the latest minimally invasive techniques, such as The Center for Innovative GYN Care’s DualPortGYN, that prevent injury to the pelvic structures and minimize blood loss – resulting in reduced complication rates and improved recovery times compared to other types of hysterectomy.
HAS THE PHYSICIAN FELLOWSHIP TRAINED IN MINIMALLY INVASIVE GYN SURGERY?
While most OB-GYNs are highly trusted generalists, they spent most of their time focusing on obstetrics and basic GYN care and therefore, perform hysterectomy and other specialized GYN surgeries rarely. Be sure to choose a surgeon who has received comprehensive training and performs many minimally invasive hysterectomies each year.
WILL THE PHYSICIAN USE POWER MORCELLATION TO REMOVE TISSUE DURING THE SURGERY?
This is an important question when considering a hysterectomy. The reason is because hidden uterine cancer called sarcoma can be spread through the abdomen and pelvis during surgery when the small motorized blades in these devices spin at high speed to cut the fibroids into small strips for removal. The Food and Drug Administration (FDA) now requires all surgeons to tell women in advance if the surgery involves a power morcellator and to get written consent before the surgery takes place. Today, new minimally invasive surgical options are available that do not involve power morcellation, such as DualPortGYN.
WILL THE PHYSICIAN USE ROBOTICS TO ASSIST WITH THE SURGERY?
Although the American Medical Association and other leading medical societies have issued statements discouraging robotic techniques due to dramatically higher costs to patients without any medical advantages, robotics continue to be used in hysterectomy and other GYN surgeries. This is because robotic procedures “enable” an OB-GYN not well trained in laparoscopic GYN surgical techniques to complete a hysterectomy through a “minimally invasive” approach. This is why women need to ask if robotics will be used during a GYN surgery and to seek a specially trained surgeon able to perform the latest minimally invasive surgical techniques, such as DualPortGYN and retroperitoneal dissection that do not use robotics.
WHAT IS MY ANTICIPATED RECOVERY TIME?
New minimally invasive techniques require, on average, only a week to recover. Other procedures such as open abdominal surgery can take up to 8 weeks.
WHAT ARE MY OTHER SURGICAL OPTIONS?
Ask your physician if he or she is aware of new, minimally invasive procedures.
Women need to be their own best advocate, which is why getting a second opinion is always good practice. Since there are different surgical options for treating fibroids, getting a second opinion is a way you can ask questions about how the surgery will be performed, the recovery time, and possible complications.
Hear About Heidi’s Story to Learn More About New Advances in Hysterectomy
(1) CDC. (2010). National Hospital Discharge Survey. Procedures by selected patient characteristics – Number by procedure category and age.


